Appeals & Prior Authorization
Streamlined prior authorization & appeals to enhance patient access to necessary therapies
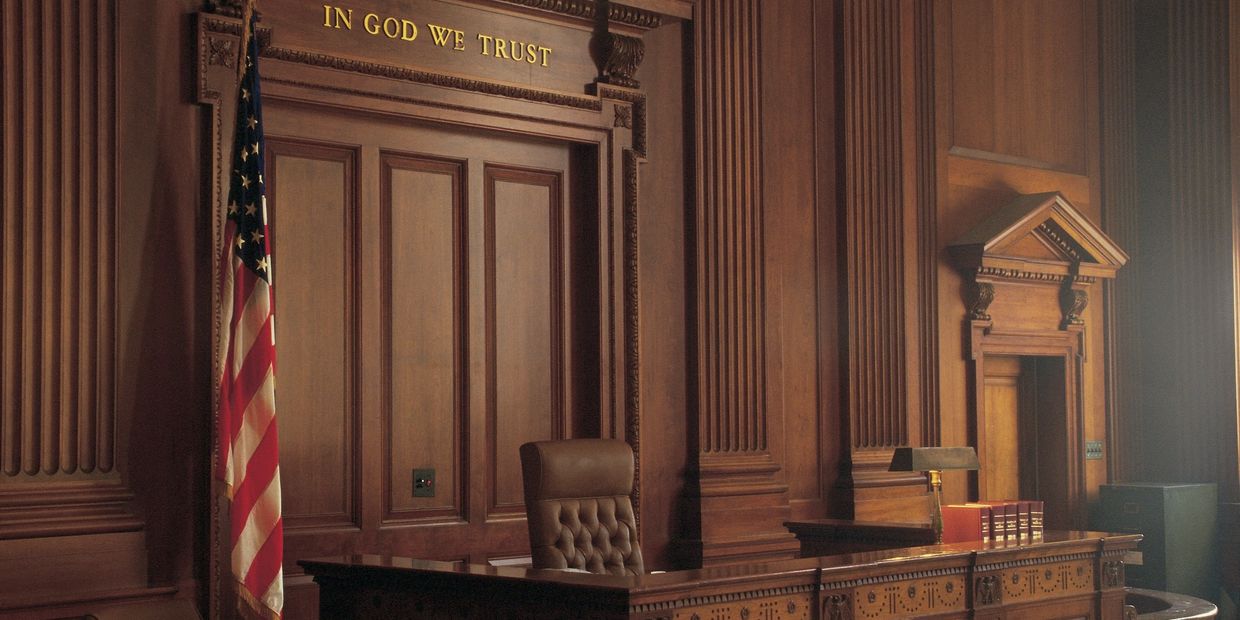
Prior authorization can make access to new treatments challenging for patients. We work with you and healthcare providers to get these treatments into the hands of patients as efficiently as possible. From benefits verification to appeals to ALJ hearings, we bridge the gap between your company, health workers, and payers to support patients and get them the treatments they need. Let's work together to help people get better with better access to innovative treatments.
Our Services
Expert guidance throughout the prior authorization process and simplification of the appeals process. We facilitate communication between healthcare providers, insurers, and patients. We manage documentation and negotiations efficiently. We navigate healthcare system challenges to fast-track treatment access. All leading to boosts in patient health outcomes and satisfaction.
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.